The chemist and druggist, 18/25. December 2010 (issue 6778)
18/36
- Publication/creation
- London : Morgan Brothers, 1859-
- Contributors
- United Business Media.
- Copyright note
- UBM.
- Type/technique
-
Electronic journals
Periodicals
- Subjects
-
Pharmacy
Drug Industry
Great Britain
- Attribution and usage
-
Wellcome Collection
You have permission to make copies of this work under a Creative Commons, Attribution, Non-commercial license.
Non-commercial use includes private study, academic research, teaching, and other activities that are not primarily intended for, or directed towards, commercial advantage or private monetary compensation. See the Legal Code for further information.
Image source should be attributed as specified in the full catalogue record. If no source is given the image should be attributed to Wellcome Collection.
The image contains the following text:
%JfU
CLINICAL
ZONE
▼19 Eczema: part 2
CLINICAL
^ 21 Pharmacokinetics
BUSINESS
^ 26 Category M
Eczema: part 2
The treatment options and stepped-care
management of eczema
Supported by
GENUS PHARMACEUTICALS
Chinjal Patel MRPharmS PCDip
The management of eczema involves the early
identification and avoidance of triggers and the
implementation of a stepped-care approach to
treatment, as recommended by Nice.1 This means
increasing treatment when the condition is severe
and reducing it when a flare is controlled.
First-line treatments include emollient therapy,
topical corticosteroids and anti-infective agents.
Other treatments include topical tar and
antimicrobial products, topical calcineurin
inhibitors, phototherapy, systemic treatment,
bandages and medicated dressings.
Emollients are the mainstay of eczema
management. They restore the epidermal barrier
and prevent the skin from becoming dry.
Common ingredients include liquid and white
soft paraffin. Emollients are available in several
forms, including creams (the most acceptable form
to patients), ointments (most effective, but messy)
and lotions (for mild dryness on the scalp and
hairy areas).
Bath emollients and emollient shower gels
should be used as an adjunct to standard topical
emollients. Soap substitutes such as emulsifying
ointment are recommended, as soap can remove
natural oils and cause the skin to become dry and
shed further skin cells.
Emulsifying ointment is effective in treating
cradle cap in babies.
Topical emollients should be smoothed onto the
skin using downward strokes in the direction of hair
growth, as rubbing them in can increase the risk of
folliculitis. They should be used liberally all over
the body as frequently as needed to prevent
eczema flare-ups.
There is no specific ranking order of emollients,
and choice is mainly down to the site and severity
of the condition and patient preference. Often
several different emollient preparations are used
together to achieve optimal management, which is
known as complete emollient therapy.
Some excipients and preservatives in emollients
may be potential irritants, such as fragrances and
benzyl alcohol. A list of potential sensitising
excipients is found in the BNF.2
Although aqueous cream is commonly used in
eczema management, it has been found to cause
skin irritation (possibly due to containing the skin
sensitisers sodium lauryl sulfate and chlorocresol).
It should therefore not be recommended as a
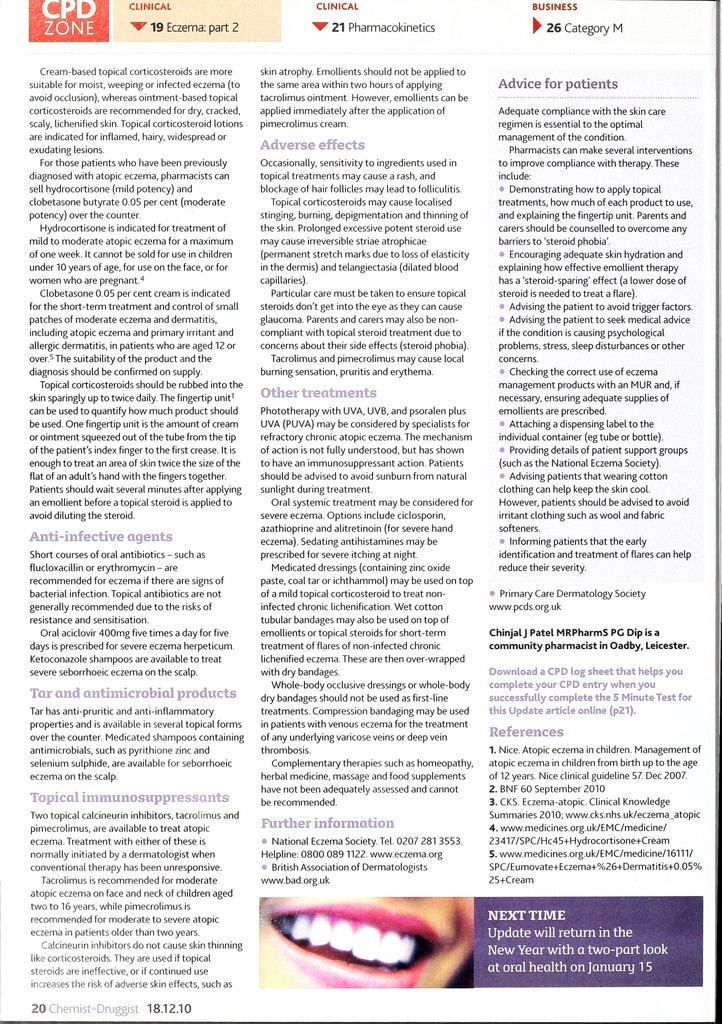
Table 1: Topical corticosteroid
potencies
MILD eg hydrocortisone 0.1-2.5 per cent (for
mild eczema, especially on the face and neck)
MODERATE eg betamethasone valerate
0.025 per cent, clobetasone butyrate 0.05
per cent (for moderate eczema)
POTENT eg betamethasone valerate 0.1 per
cent (for severe eczema)
VERY POTENT eg clobetasol propionate
0.05 per cent (should only be used under
specialist dermatological advice)
leave-on moisturiser. All emollients should be
patch-tested before use on large or sensitive areas.
Emollients should be prescribed in large
quantities. Typical amounts used weekly are 600g
for adults and 250g for children.3 CPs may
prescribe adjuvant emollients to treat secondary
conditions in the skin.
Emollients may also contain:
antimicrobials, such as triclosan for widespread
or recurrent infection
- lauromacrogols, for their anaesthetic and hence
anti-itching properties
salicylic acid, for when an exfoliating action is
needed
colloidal oatmeal, for its soothing, anti-itching
properties
humectants, such as urea and glycerine. These
provide extra hydration by drawing water from the
dermis into the epidermis.
It is important to review emollient therapy, as
the effectiveness and acceptability of an emollient
can vary with time.
Topical corticosteroids
Topical corticosteroids are another mainstay in
the treatment of eczema. They relieve
inflammation and itching by inhibiting
inflammatory mediators. Topical corticosteroids
are categorised in the BNF2 into four groups of
potency, and the least potent preparation which
effectively controls the condition should always
be used.
Topical corticosteroids are the first-line
treatment for flares of atopic eczema. The choice is
based on the potency of the product and site and
severity of the eczema. See table 1, above, for
details.